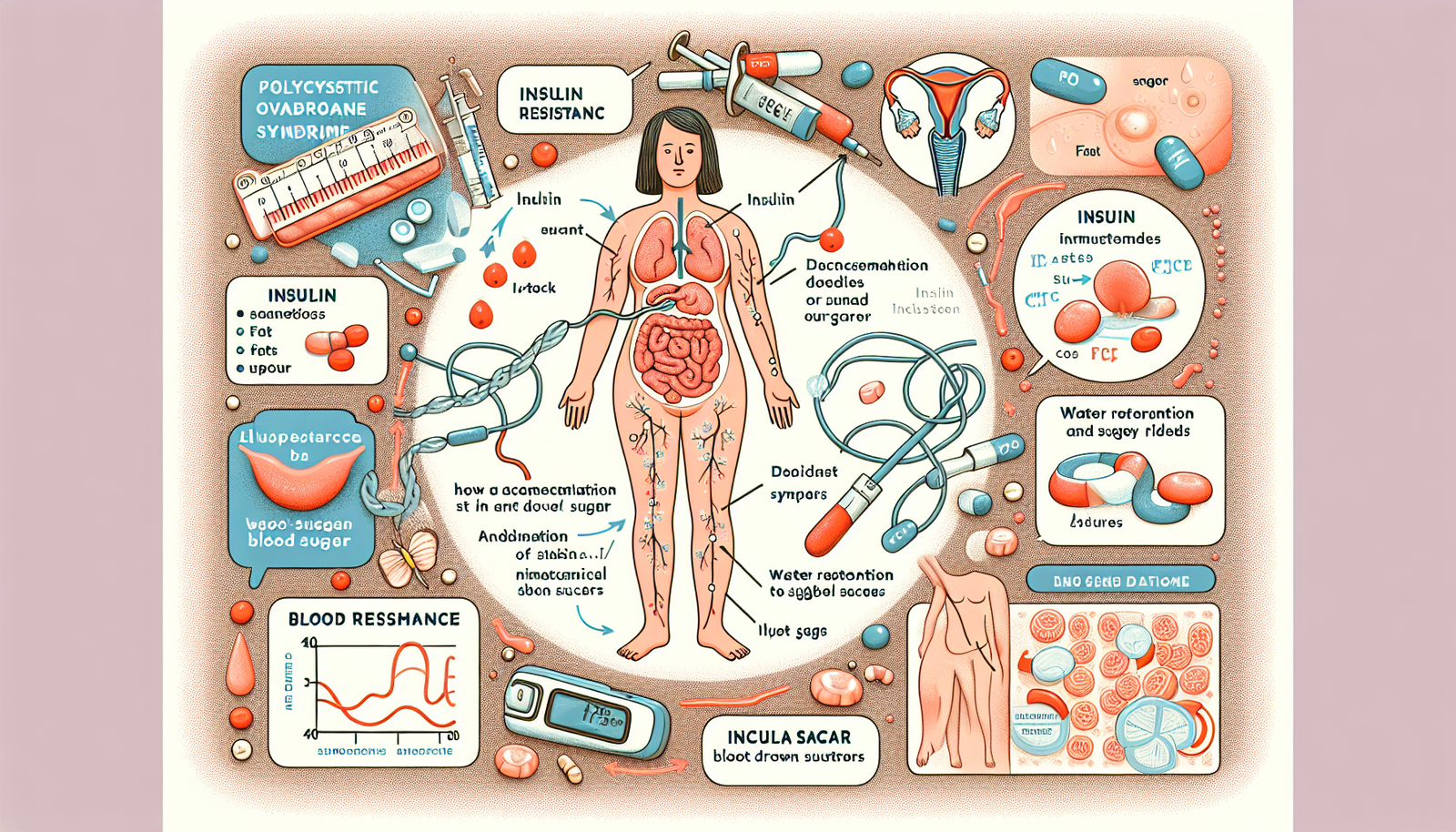
Polycystic Ovary Syndrome (PCOS) is hormonal disorder that affects significant number of women worldwide. One of the key components of PCOS is insulin resistance; this can significantly hinder weight loss efforts and lead to several health complications. However, this post dives deep into the symptoms of insulin resistance associated with PCOS, effective treatment strategies and lifestyle changes that can help manage this condition. Although many women struggle with these challenges, understanding their impact is crucial for better health outcomes. Because of the complexity of PCOS, it is essential to explore various avenues for support and management.
What is Insulin Resistance?
Insulin resistance (which occurs when body’s cells become less responsive to insulin) is a condition characterized by decreased cellular response to a hormone that plays a crucial role in blood sugar control. When insulin functions properly, it allows sugar from bloodstream to enter cells (to be used for energy). However, with insulin resistance, cells do not respond effectively to insulin, leading to elevated blood sugar levels and increased insulin production. This condition is particularly prevalent among women (with PCOS), because reports indicate that around 80% of women with this syndrome struggle with insulin resistance.
When insulin resistance (if left unmanaged) can lead to weight gain, this can also increase the risk of developing type 2 diabetes and other metabolic disorders. Understanding (the symptoms associated with insulin resistance) is crucial for early detection and management; however, many overlook these signs. Although it may seem negligible at first, ignoring them can have serious consequences. Because of this, recognizing the indicators becomes essential for maintaining health in the long run.
Symptoms of Insulin Resistance in PCOS
Here (are) some common signs (and) symptoms that may (or) may not indicate insulin resistance: however, this condition can be subtle. Although fatigue and weight gain are frequently reported, many individuals experience (other) less obvious indicators. Because insulin resistance can manifest in diverse ways, it is crucial to recognize these signs. Increased hunger may also occur, but it often goes unnoticed, leading to further complications. In conclusion, understanding these signals is essential for early intervention.
- Weight Gain: Particularly in the abdominal area, insulin resistance can lead to fat being stored around the organs, making it difficult to lose belly fat.
- Swollen Ankles, Feet, or Hands: Insulin’s role in kidney function can lead to water retention, causing swelling in the extremities.
- Post-Meal Hunger and Sugar Cravings: If you find yourself reaching for sweets after meals, it might be due to your body not effectively utilizing the energy from your food.
- Dark Skin Patches and Skin Tags: High insulin levels can result in dark patches of skin, often found in areas like the neck or armpits.
- Frequent Urination and Extreme Thirst: Elevated blood sugar levels can lead to increased urination and thirst as the body tries to eliminate excess sugar.
- Irregular Menstrual Cycles: High insulin levels can cause hormonal imbalances leading to irregular periods.
- Elevated Blood Sugar Levels: Monitoring blood sugar levels can help identify insulin resistance; a failure to return to baseline after meals may indicate a problem.
Understanding the Link Between PCOS and Insulin Resistance
For women (dealing) with PCOS, insulin resistance can exacerbate symptoms (that) are associated with the condition. High insulin levels can trigger the ovaries to produce more testosterone; this leads to symptoms such as hair loss, acne and anxiety. Managing insulin resistance is, however, a vital part of treating PCOS. Because of this, it can lead to an improvement in overall symptoms.
How to Manage Insulin Resistance
Fortunately, insulin resistance can be reversed with the appropriate lifestyle changes and treatments. Here are several strategies to help manage insulin resistance; however, some individuals may find it challenging. This is because, although these modifications can be effective, they often require considerable dedication and effort. But it is essential to remain committed, as the benefits can be substantial.
- Eat Less Foods That Spike Blood Sugar: Focus on a balanced diet that includes carbohydrates, proteins, and fats. Pairing carbs with protein and healthy fats can help stabilize blood sugar levels.
- Reduce Meal Frequency: Eating fewer meals throughout the day can help keep insulin levels lower. Aim for three meals and one or two healthy snacks if needed.
- Consider a Gluten-Free Diet: Some women find that gluten can cause inflammation and exacerbate insulin resistance. Eliminating gluten for 30 days can help determine its impact on your symptoms.
- Try Going Dairy-Free: Dairy products can raise insulin levels, so cutting them out might help improve insulin sensitivity.
- Modify Your Exercise Routine: Instead of long cardio sessions, focus on strength training and short bursts of high-intensity workouts to improve insulin sensitivity.
- Prioritize Sleep: Aim for quality sleep, as inadequate sleep can worsen insulin resistance. Studies show that even one week of poor sleep can significantly impact insulin sensitivity.
- Manage Stress Levels: Chronic stress can lead to elevated blood sugar levels. Incorporate stress-reducing practices like yoga, meditation, or journaling into your daily routine.
One Easy Daily Tip to Improve Insulin Resistance
A simple (yet effective) method to enhance insulin sensitivity is to take walk after meals. Research indicates that light physical activity—such as walking—can significantly help lower insulin levels and improve blood sugar control. Making this a habit can lead to better management of insulin resistance; however, it can also alleviate overall PCOS symptoms. Although it may seem trivial, this practice is beneficial because it promotes a healthier lifestyle.
Supplementing for Success
In addition to lifestyle changes, certain supplements (such as Ovasitol) can aid in managing PCOS and insulin resistance; however, one such supplement has been reported to help many women regulate their menstrual cycles and reduce cravings. It works at a cellular level to address the root causes of insulin resistance, making it a valuable addition to your routine. Although some may be skeptical, this supplement proves beneficial because it targets underlying issues. Insulin resistance is complex, but Ovasitol’s effectiveness is noteworthy.
FAQs
Can insulin resistance be reversed?
Indeed, insulin resistance (1) can be reversed through lifestyle changes, dietary adjustments and sometimes (2) supplements. Regular exercise is crucial, as are balanced diets and stress management; these are key components in reversing insulin resistance. However, achieving this requires commitment and (3) consistency. Although some may find it challenging, the benefits are undeniable.
How does PCOS affect weight loss?
PCOS (polycystic ovary syndrome) can make weight loss more challenging because of insulin resistance and hormonal imbalances that promote fat storage. However, managing insulin resistance through diet and exercise can significantly improve weight loss efforts; this is crucial for those affected. Although it may be difficult, individuals often find success when they commit to lifestyle changes. But, it requires persistence and dedication.
What dietary changes should I make if I have PCOS?
Focus on diet rich in whole foods (including vegetables, lean proteins, healthy fats and whole grains). Limit processed foods (sugar and refined carbohydrates), because this helps stabilize blood sugar levels. However, one must be cautious, because these changes can be challenging. Although it may seem difficult, the benefits significantly outweigh the drawbacks.
Are there specific exercises that help with PCOS?
Strength training and high-intensity interval training (HIIT) are particularly effective (for improving insulin sensitivity). However, it’s essential to incorporate regular physical activity into (your) routine, because this can enhance overall health. Although some may find it challenging, the benefits are numerous.
Is it necessary to take supplements for PCOS?
While not every needs supplements, they can be beneficial (for some women) with PCOS. Ovasitol—(for example)—has shown promise in improving insulin sensitivity; however, it also plays a role in regulating menstrual cycles.
Conclusion
Managing insulin resistance is crucial for women with PCOS. By recognizing the symptoms (however), implementing lifestyle changes and considering supplements, you can take control of your health and improve your quality of life. Remember: it’s not just about managing PCOS; it’s about thriving in your health journey, although this may require perseverance and dedication.